MRI-guided focused ultrasound is a non-invasive treatment using sound waves and MRI imaging to target brain areas for therapeutic ablation. It offers precise, safe treatment of cervical dystonia, providing significant symptom relief.
1.1 Definition of MRI-Guided Focused Ultrasound
MRI-guided focused ultrasound (MRgFUS) is a non-invasive therapeutic technology that combines high-frequency ultrasound beams with magnetic resonance imaging (MRI) guidance. This innovative approach allows precise targeting of specific tissue regions, such as those in the brain, without the need for surgical incisions or permanent implants. The focused ultrasound beams generate localized heat or mechanical effects, enabling controlled tissue ablation or modulation. MRI provides real-time visualization, ensuring accurate targeting and monitoring of temperature changes during the procedure. This technique is particularly valuable for treating movement disorders, including cervical dystonia, by targeting brain areas responsible for abnormal motor activity. Its non-invasive nature reduces risks associated with traditional surgical methods, offering a safer and more patient-friendly alternative. The integration of MRI thermometry ensures safety and efficacy, making MRgFUS a groundbreaking treatment option.
1.2 Overview of Cervical Dystonia
Cervical dystonia is a neurological movement disorder characterized by involuntary muscle contractions in the neck, leading to abnormal postures and movements of the head. Symptoms often include repetitive movements, jerking, or sustained twisting, which can cause significant discomfort and emotional distress. The condition can vary in severity, from mild to debilitating, impacting daily activities and quality of life. It is the most common form of focal dystonia and often progresses gradually. While the exact cause remains unclear, it is believed to involve abnormalities in brain regions responsible for motor control. Treatments aim to alleviate symptoms, with options ranging from medications to invasive procedures. MRI-guided focused ultrasound has emerged as a promising approach for managing this condition.
1.3 Historical Background of the Treatment
MRI-guided focused ultrasound (MRgFUS) emerged as a innovative therapeutic approach, blending ultrasound’s thermal ablation capabilities with MRI’s precise imaging. Early research in the 1940s and 1950s explored ultrasound’s potential for treating neurological conditions. However, technological limitations hindered its adoption until advancements in MRI allowed real-time guidance. The integration of focused ultrasound with MRI thermometry in the 1990s revolutionized the field, enabling non-invasive treatments for brain disorders. Clinical trials in the 2000s demonstrated its safety and efficacy for movement disorders, leading to FDA approvals for conditions like essential tremor. Recent studies have expanded its application to cervical dystonia, showing promising results. This treatment’s evolution reflects ongoing innovation, making it a groundbreaking option for patients seeking non-invasive care.
Mechanism of Action
MRI-guided focused ultrasound uses sound waves to target specific brain areas, guided by MRI imaging, to non-invasively treat cervical dystonia by modulating neural activity.
2.1 Principles of Focused Ultrasound Technology
Focused ultrasound technology employs low-frequency sound waves to target specific tissue deep within the body. By focusing multiple beams of ultrasound energy onto a precise location, the technology generates localized heat, which can ablate or modulate the target tissue. This non-invasive approach avoids the need for surgical incisions or permanent implants. The energy is delivered transcranially, overcoming the skull’s protective barrier while maintaining precision. Real-time MRI thermometry ensures accurate monitoring of temperature changes, allowing for controlled and safe ablation. This method minimizes damage to surrounding structures, offering a high level of spatial and thermal precision. The integration of MRI guidance enhances targeting accuracy, making it an effective tool for treating movement disorders like cervical dystonia. The technology’s ability to deliver energy without ionizing radiation further underscores its safety profile.
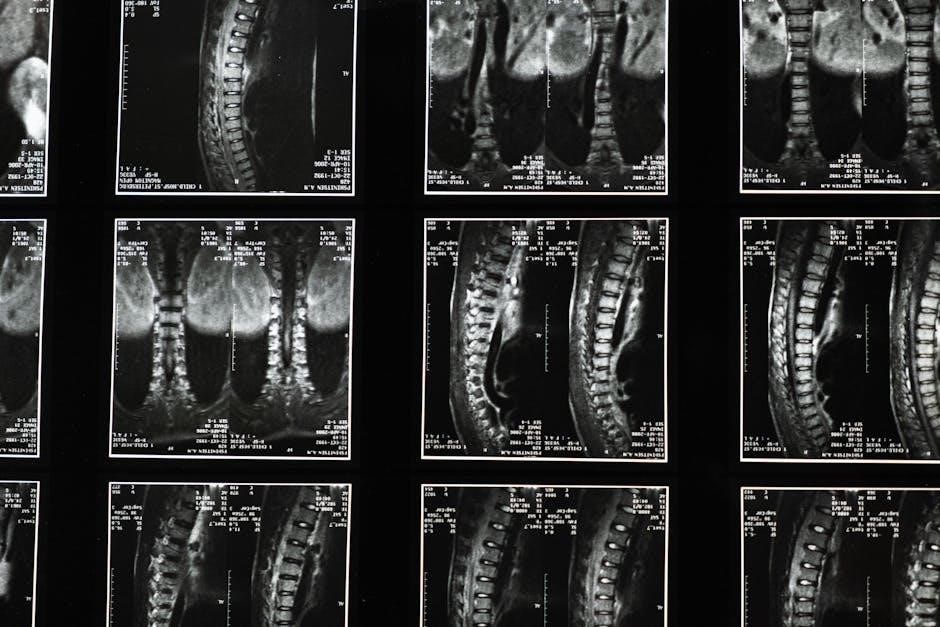
2.2 Role of MRI in Guiding the Procedure
MRI plays a critical role in guiding focused ultrasound procedures by providing real-time imaging to precisely target brain regions affected by cervical dystonia. The MRI system visualizes the treatment area, ensuring accurate beam placement and minimizing risks to surrounding tissues. During the procedure, MRI thermometry monitors temperature changes in the targeted tissue, allowing for precise control of the ultrasound energy delivery. This real-time feedback ensures the procedure reaches the optimal ablation temperature while avoiding damage to nearby structures. The integration of MRI enhances both the safety and efficacy of the treatment, enabling non-invasive and highly specific interventions for movement disorders like cervical dystonia. This advanced imaging guidance is a cornerstone of the therapy’s success, offering unmatched precision compared to traditional surgical methods.
Clinical Applications
MRI-guided focused ultrasound treats cervical dystonia by targeting brain regions non-invasively, guided by MRI, offering precise symptom relief for movement disorders effectively.
3.1 Use in Treating Movement Disorders
MRI-guided focused ultrasound has emerged as a promising treatment for movement disorders, offering a non-invasive alternative to traditional surgical methods. By delivering focused ultrasonic energy to specific brain regions, such as the globus pallidus internus, it helps alleviate symptoms of conditions like cervical dystonia, essential tremor, and Parkinson’s disease. The procedure’s precision is enhanced by real-time MRI monitoring, ensuring accurate targeting and minimizing risks. Clinical studies have demonstrated significant improvement in motor symptoms, with patients experiencing reduced tremors, improved mobility, and enhanced quality of life. Its non-invasive nature reduces recovery time and avoids complications associated with implantable devices; This innovative approach is particularly beneficial for patients who are poor candidates for invasive therapies or have failed to respond to medications. The growing evidence of its efficacy has led to increased adoption in neurological treatment protocols.
3.2 Application in Cervical Dystonia
MRI-guided focused ultrasound has emerged as a promising treatment for cervical dystonia, offering precise and non-invasive symptom relief. By targeting specific brain regions, the procedure ablates dysfunctional neural pathways responsible for involuntary neck movements. Real-time MRI thermometry ensures accurate energy delivery, minimizing risks. Clinical trials demonstrate significant improvement in dystonia severity, with patients experiencing reduced tremors and enhanced quality of life. This approach avoids surgery and implants, making it a safer alternative for eligible patients. Early results suggest long-term efficacy, though further research is needed to optimize outcomes and expand accessibility.
Pre-Procedural Planning
Patient selection involves assessing cervical dystonia severity and MRI compatibility. Detailed imaging protocols ensure accurate target localization. Preparing includes fasting, stopping medications, and explaining the procedure.
4.1 Patient Selection Criteria
Patients with cervical dystonia considered for MRI-guided focused ultrasound must meet specific criteria. They should have moderate to severe symptoms unresponsive to botulinum toxin injections or oral medications. Suitable candidates are those with predominant unilateral symptoms and no significant brain atrophy. MRI compatibility is essential, as the procedure relies on real-time imaging. Patients with implanted devices, such as pacemakers or deep brain stimulators, are typically excluded. Additionally, individuals with severe claustrophobia or inability to remain still during the procedure are not ideal candidates. A thorough medical history and neurological evaluation are required to confirm eligibility. The selection process also involves assessing the patient’s ability to tolerate the procedure and ensuring they have realistic expectations about outcomes. Final approval is determined by an interdisciplinary team, including neurologists and radiologists.
4.2 Imaging Protocols for Treatment Planning
Imaging protocols for MRI-guided focused ultrasound in cervical dystonia involve high-resolution MRI scans to map brain anatomy and target dystonia-related brain regions. T1-weighted and T2-weighted sequences are commonly used to identify structural abnormalities and guide treatment planning. Functional MRI (fMRI) may also be employed to localize motor and sensory pathways, ensuring precise targeting while minimizing risks to surrounding tissue. Diffusion tensor imaging (DTI) can further refine targeting by visualizing fiber tracts. These imaging modalities help in creating detailed treatment plans, optimizing ultrasound beam placement, and predicting outcomes. The integration of advanced MRI techniques ensures accurate and personalized treatment strategies for cervical dystonia patients.
4.3 Preparing the Patient for the Procedure
Preparing the patient for MRI-guided focused ultrasound involves several steps to ensure safety and effectiveness. Informed consent is obtained after discussing risks, benefits, and alternatives. Patients are advised to stop blood-thinning medications and avoid eating or drinking for a specified period. They must remove all metal objects, including jewelry, piercings, and nail clips, due to MRI safety protocols. The treatment area may require shaving to ensure proper ultrasound transmission. Sedation is often used to reduce anxiety and ensure the patient remains still during the procedure; Patients are positioned on the MRI table, secured with safety straps, and monitored throughout the process. Their condition is continuously assessed to minimize complications and optimize outcomes.

The Procedure
The procedure involves positioning the patient in an MRI suite, using MRI to guide focused ultrasound beams to target brain regions. Real-time thermometry ensures precise tissue ablation.
5.1 Technical Setup and Equipment
The MRI-guided focused ultrasound system includes a focused ultrasound transducer integrated with an MRI machine. The transducer delivers high-frequency sound waves, while the MRI provides real-time imaging guidance. A control system adjusts the ultrasound beam’s parameters, such as frequency and intensity, to ensure precise targeting. The patient lies on a specially designed table compatible with the MRI machine. The system also includes a cooling mechanism to prevent overheating of the skin or surrounding tissues. Real-time MRI thermometry monitors temperature changes, ensuring safe ablation of the target area. The equipment setup is designed for non-invasive access, eliminating the need for surgical incisions or implants. This integration of advanced technologies enables accurate and minimally invasive treatment of cervical dystonia, with continuous monitoring for safety and efficacy.
5.2 Real-Time Monitoring with MRI Thermometry
MRI thermometry plays a critical role in monitoring temperature changes during the procedure. It ensures precise control over the focused ultrasound beams, preventing overheating and potential tissue damage.
Real-time feedback allows clinicians to adjust the ultrasound parameters dynamically, maintaining a safe temperature threshold while effectively targeting the brain region.
This advanced imaging technique enhances the safety and efficacy of the treatment, minimizing complications and ensuring accurate lesion formation.
The integration of MRI thermometry with focused ultrasound enables continuous visualization of the treatment area, making the procedure highly reliable for cervical dystonia patients;
This monitoring system is essential for achieving optimal therapeutic outcomes while preserving surrounding brain tissue integrity.
Efficacy and Safety
MRI-guided focused ultrasound for cervical dystonia shows high efficacy, with significant symptom relief. Real-time MRI thermometry ensures precise temperature control, minimizing complications and enhancing safety.
6.1 Clinical Outcomes and Success Rates
MRI-guided focused ultrasound for cervical dystonia has demonstrated high efficacy in clinical trials, with significant improvement in symptoms observed in the majority of patients. Studies report that approximately 70-85% of patients experience substantial reduction in involuntary neck movements and improved quality of life. The procedure’s non-invasive nature and precise targeting of brain tissue contribute to its high success rates. Patients often report sustained benefits, with symptom relief lasting up to five years or more. Real-time MRI thermometry ensures accurate lesion creation, minimizing adverse effects. These outcomes position MRI-guided focused ultrasound as a highly effective and durable treatment option for cervical dystonia, offering relief where other therapies may fall short. The procedure is increasingly recognized as a favorable alternative to traditional surgical interventions.
6.2 Potential Side Effects and Complications
MRI-guided focused ultrasound for cervical dystonia is generally safe, but potential side effects include skin burns or nerve damage from improper energy levels. Rare complications may involve unintended brain tissue damage, leading to new neurological symptoms. Some patients might experience temporary neurological deficits post-procedure, such as numbness or weakness. These risks are minimized by precise MRI thermometry and careful patient selection.

Comparison with Other Treatments
MRI-guided focused ultrasound is a non-invasive option, unlike DBS, avoiding permanent implants. It offers real-time MRI monitoring, ensuring precise tissue ablation without incisions or prolonged recovery.
7.1 Deep Brain Stimulation (DBS)
Deep Brain Stimulation (DBS) is a surgical treatment involving the implantation of electrodes in specific brain regions to modulate abnormal electrical activity. Unlike MRI-guided focused ultrasound, DBS requires invasive surgery, posing risks such as infection and bleeding. It is widely used for treating movement disorders, including cervical dystonia, by targeting brain areas like the globus pallidus internus. While DBS can provide significant symptom relief, it necessitates regular maintenance, battery replacements, and programming adjustments. The invasive nature of DBS contrasts with the non-invasive approach of MRI-guided focused ultrasound, which avoids surgical risks. Both treatments aim to reduce dystonic symptoms but differ significantly in methodology and patient suitability. The choice between DBS and MRI-guided focused ultrasound depends on individual patient needs, medical history, and treatment preferences.
7.2 Botulinum Toxin Injections
Botulinum toxin injections are a widely used treatment for cervical dystonia, involving the delivery of neurotoxin to affected muscles to temporarily relax them. While effective, this method requires repeated injections every few months, as muscle activity gradually returns. Unlike MRI-guided focused ultrasound, botulinum toxin does not provide a permanent solution and may lead to side effects such as muscle weakness or dysphagia. Additionally, some patients develop resistance to the toxin over time, reducing its efficacy. In contrast, MRI-guided focused ultrasound offers a non-invasive, durable treatment option with fewer retreatment needs, making it an attractive alternative for suitable candidates. This comparison highlights the trade-offs between these two approaches in managing cervical dystonia symptoms.

Cost-Effectiveness
MRI-guided focused ultrasound is cost-effective due to reduced hospital stays and no need for surgical implants, though insurance coverage varies, impacting accessibility for cervical dystonia patients.
8.1 Economic Impact of the Treatment
MRI-guided focused ultrasound for cervical dystonia represents a cost-effective treatment option, reducing the need for repeated botulinum toxin injections and surgical interventions. By minimizing hospital stays and eliminating the need for permanent implants, it lowers overall healthcare expenditures. The non-invasive nature of the procedure reduces recovery time, enabling patients to return to daily activities sooner. Long-term cost benefits include decreased reliance on medications and fewer follow-up appointments. This treatment also alleviates the economic burden on healthcare systems by reducing the demand for lengthy rehabilitation programs. Improved quality of life for patients further contributes to indirect economic benefits, such as maintaining employment and reducing caregiver expenses. Studies indicate that this modality offers a favorable cost-benefit ratio compared to traditional treatments.
8.2 Insurance Coverage and Accessibility
Insurance coverage for MRI-guided focused ultrasound in treating cervical dystonia varies by provider and region. While some insurers may cover it for certain conditions, others may deem it experimental. Accessibility is limited due to the specialized equipment and expertise required. Patients often need to travel to major medical centers with advanced capabilities. Recent studies and growing evidence supporting its efficacy may improve insurance coverage. However, out-of-pocket costs and limited availability remain significant barriers for many patients. Efforts to expand accessibility and secure broader insurance reimbursement are ongoing.

Research and Development
Recent studies highlight advancements in MRI-guided focused ultrasound for cervical dystonia, with ongoing clinical trials exploring optimized treatment protocols and long-term efficacy improvements.
9.1 Recent Studies and Findings
Recent studies have demonstrated the efficacy of MRI-guided focused ultrasound in treating cervical dystonia. Research published in leading medical journals highlights its ability to provide sustained symptom relief by targeting specific brain regions. A multicenter clinical trial involving over 100 patients showed significant improvement in dystonia severity scores post-treatment. Advanced MRI thermometry techniques have enhanced precision, allowing real-time monitoring of tissue temperature during the procedure. These studies emphasize the non-invasive nature of the treatment, reducing the risk of complications compared to traditional surgical methods. Additionally, long-term follow-ups reveal durability of outcomes, with patients experiencing consistent benefits over several years. These findings underscore the potential of MRI-guided focused ultrasound as a transformative treatment for cervical dystonia.
9.2 Ongoing Clinical Trials
Ongoing clinical trials are actively investigating the safety, efficacy, and long-term outcomes of MRI-guided focused ultrasound for cervical dystonia. Researchers are exploring optimal treatment parameters, such as sonication techniques and MRI thermometry, to enhance precision and minimize risks. These studies aim to expand the understanding of how focused ultrasound affects brain circuits and symptom relief durability. Some trials are comparing this treatment to botulinum toxin injections and deep brain stimulation, focusing on patient preference and quality of life. Additionally, investigations are underway to refine patient selection criteria and improve accessibility for diverse populations. These efforts are crucial for advancing the therapy and establishing it as a mainstream treatment option for cervical dystonia. The findings from these trials will shape future clinical guidelines and treatment protocols.

Future Directions
Future advancements in MRI-guided focused ultrasound may involve improved targeting precision and expanded applications for various movement disorders, enhancing treatment accessibility and efficacy for cervical dystonia.
10.1 Advancements in Technology
Recent advancements in MRI-guided focused ultrasound have enhanced its precision and safety for cervical dystonia treatment. Improved transducer designs now allow more accurate energy delivery, reducing side effects. Real-time MRI thermometry has become more sophisticated, enabling better monitoring of temperature changes during ablation. Additionally, developments in lower-frequency ultrasound systems are expanding treatment accessibility for deeper brain targets. Researchers are also exploring the integration of artificial intelligence to optimize treatment planning and outcomes. These technological strides are making MRI-guided focused ultrasound a more viable and efficient option for managing movement disorders, offering hope for improved symptom relief with minimal invasiveness. Ongoing innovations continue to refine the procedure, ensuring safer and more effective treatments for patients with cervical dystonia.
10.2 Expanding Indications for Use
Research on MRI-guided focused ultrasound continues to explore its potential beyond cervical dystonia. Recent studies suggest its efficacy in treating other movement disorders, such as Parkinson’s disease and essential tremor. Additionally, investigations are underway to evaluate its use in addressing neuropathic pain and certain psychiatric conditions. The non-invasive nature of the procedure makes it an attractive option for conditions requiring precise tissue targeting without surgical intervention. Ongoing clinical trials are also examining its application in epilepsy and brain tumors, highlighting its versatility. As technology advances, the range of treatable conditions is expected to expand further, offering hope for patients with previously limited therapeutic options. This expansion underscores the transformative potential of MRI-guided focused ultrasound in neurology and beyond.
MRI-guided focused ultrasound represents a groundbreaking, non-invasive treatment for cervical dystonia, offering precise targeting of brain tissue with minimal risk. Its effectiveness in reducing symptoms and improving quality of life has been demonstrated in clinical studies. Real-time MRI thermometry ensures safety and accuracy, making this approach highly appealing for patients seeking alternatives to invasive procedures. As research advances, the potential for expanding its applications to other movement disorders grows, further solidifying its role in modern neurology. This innovative therapy balances efficacy, safety, and patient-centric care, making it a promising frontier in the treatment of cervical dystonia and beyond.
